The liver is a slacker. It toils hour after hour without requiring thanks. It filters poisons. It processes nutrients. It produces energy. But sometimes fat accumulates in this workhorse organ. That’s hepatic steatosis.
Fatty liver disease, or hepatic steatosis, is the most prevalent liver illness across the globe presently. It generally occurs slowly and quietly in most people. No signs may initially be evident. It can eventually affect health over the course of many years.
Here in this book, we will be discussing what hepatic steatosis is, why it happens, its risk, and how it’s being treated. Knowledge is the start of prevention. And action is the step which guarantees your future.
What is Hepatic Steatosis
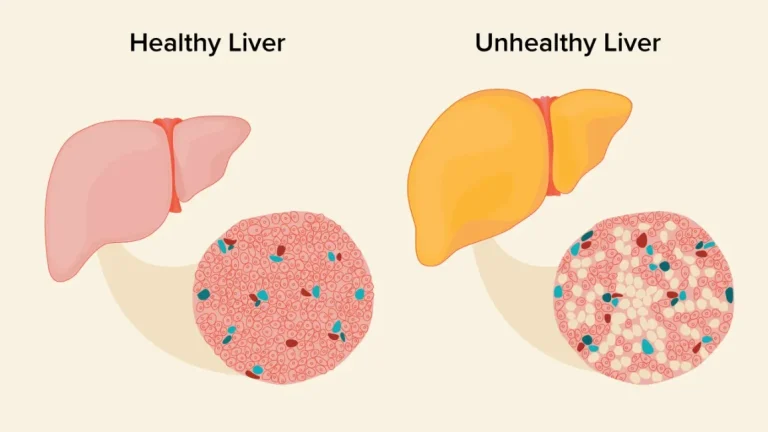
Hepatic steatosis is the stored fat within the liver. The liver of a healthy individual holds little or no fat. But the instant additional fat is 5 to 10 percent of the liver, doctors call it fatty liver disease.
Two Main Types
Alcoholic fatty liver disease (AFLD): Due to excessive alcohol use.
Nonalcoholic fatty liver disease (NAFLD): Without excessive alcohol use. That is the more common one today.
Either or both can worsen. Either or both can lead to liver damage if left untreated.
Causes of Hepatic Steatosis
Why is the liver fatty? The reasons are numerous.
Lifestyle Causes
Alcohol intake in excess.
Diet rich in sugars, refined carbs, and unhealthy fats.
Abdominal obesity.
Physical inactivity.
Medical Causes
Insulin resistance and diabetes.
Hypertriglyceridemia or hypercholesterolemia.
Certain drugs such as steroids.
Malnutrition or unintentional weight loss.
Genetic Factors
Family history is also another risk factor. Individuals are susceptible to fat deposition in the liver based on genetic reasons.
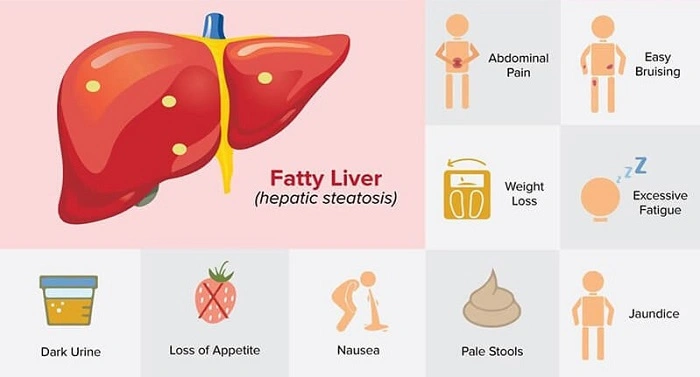
Symptoms of Hepatic Steatosis
Silence is the biggest risk. Hepatic steatosis lacks physical manifestations in early stages.
Screening Signs
Fatigue.
Right upper quadrant abdominal pain.
Unexplained weakness.
Hepatomegaly as revealed by tests.
Late Signs
Once it advances to inflammation or cirrhosis, symptoms can be:
Yellowing of skin (jaundice).
Swelling of legs or abdomen.
Bleeding easily.
Confusion due to toxin buildup.
Diagnosis of Hepatic Steatosis
Doctors use a mixture of scanning, testing, and biopsies where needed.
Tests
Blood tests: May have high liver enzymes.
Ultrasound: Delineates fat buildup.
CT or MRI scans: Precise scanning.
Liver biopsy: Establishes diagnosis and severity.
Early-phase diagnosis is crucial. Since screening is especially suited in the case of those patients with risk factors like diabetes or obesity.
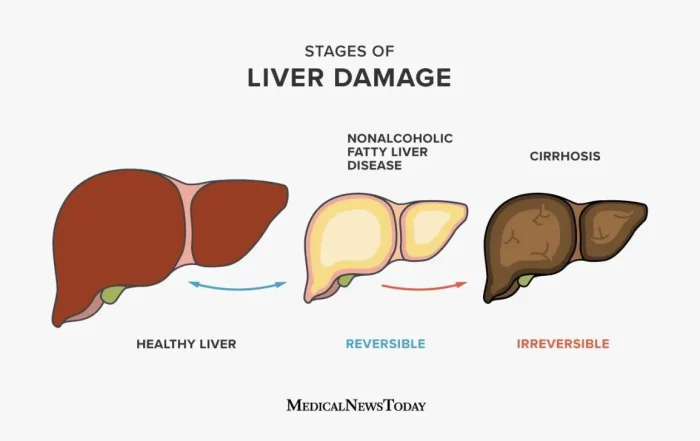
Stages of Hepatic Steatosis
Severity may not always occur with fatty liver but can evolve.
Simple Fatty Liver
Inflammation-free fat within the liver. Typically benign if addressed.
Nonalcoholic Steatohepatitis (NASH)
Fat with inflammation. Scarring can ensue.
Fibrosis
Repeated inflammation leads to scarring.
Cirrhosis
Advanced scarring. The liver becomes hardened. This phase can lead to liver failure.
Health Risks
Hepatic steatosis is more than a liver disease. It can affect overall health.
Does enhance risk for heart disease.
Linked to type 2 diabetes.
Can cause liver cancer.
Can cause cirrhosis or even liver failure.
That’s why early treatment is so important.
Treatment of Hepatic Steatosis
No magic pill for cure from fatty liver. But some functional reversal or management means.
Lifestyle changes
Weight loss: Even 5–10% weight loss is good for the liver.
Healthy diet: More veggies, lean protein, wholegrain. Less processed foods and added sugars.
Regular exercise: Leads to weight loss and insulin sensitivity.
Moderate drinking: Or better yet, abstain.
Medications
No medication for NAFLD yet. Physicians, however, may employ drugs to treat the related conditions:
Cholesterol-lowering drugs.
Drugs used to treat diabetes.
Vitamin E or antioxidants in certain circumstances.
Surgical Intervention
In obesity, especially in morbid obesity, weight loss and improvement in liver disease can be achieved by bariatric surgery.
Diet for Fatty Liver
Hepatic steatosis is treated by diet.
Recommended
Leafy vegetables and green leafy vegetables.
Fresh fruits.
Fish with omega-3 content.
Nuts and olive oil.
Whole grains.
Avoid
Sweet drinks.
Fast foods and fried food.
Excess red meat.
Processed snacks.
Alcohol.
A balanced diet forms the foundation of recovery.
Life Habits to Preserve the Liver
Exercising daily.
Getting enough sleep.
Managing stress.
Hydrating with plenty of water.
These small habits accumulate in protection.
Prevention of Hepatic Steatosis
Prevention is best.
Stay in shape, maintain a healthy weight.
Eat well-balanced, healthy foods.
Exercise daily.
Don’t binge drink.
Monitor cholesterol and blood sugar.
These rituals protect not only the liver but also the heart and body.
Living with Hepatic Steatosis
Diagnosis is not death. Most live long, healthy lives with proper care. The liver is a great healing organ. If the fat clears, the organ heals. Energy returns to patients. Mood improves. Health feels lighter.
Check-ups, support groups, and regular maintenance make the ride smoother.
Patient Stories
A male patient in his forties found he had hepatic steatosis during a check-up. He walked daily and lost 15 pounds. His blood work improved in a few months. He felt younger and more energetic.
A diabetic woman discovered she had fatty liver. She became a vegetarian and was able to control her sugar. Her doctor told her the fat in her liver was melting away. She told us that she could finally feel that she was doing something positive for her own health.
These accounts remind us that change is available.
Hepatic Steatosis and Global Health
It’s on the rise everywhere in the world. With Western diets and lack of exercise, millions are in danger. Information campaigns characterize public health today. Doctors prescribe tests for at-risk individuals. On www々, it can be averted so that one day there isn’t an epidemic of liver disease looming over our heads.
The Future of Treatment
More research is in progress. New medicines are under trial to reduce liver fat by researchers. Research might be able to tell us why some people are more likely to develop it. The possibilities exist: improved prevention and treatment in the future.
FAQs On Hepatic Steatosis
Is hepatic steatosis reversible?
Yes, change in diet, weight loss, and lifestyle modification improve it.
Can fatty liver harm?
It causes unease in the upper right quadrant in a few, but never pain in anyone.
Does alcohol always cause fatty liver?
No. Nonalcoholic fatty liver disease is a disorder in people who drink little or no alcohol.
Can hepatic steatosis happen in children?
Yes, with obesity and dietarily suspicious trends, but reversible with lifestyle change.
When should I see the doctor?
If you do have risk factors like obesity, diabetes, or cholesterol issues, you need to visit the physician for check-ups periodically.
Liver steatosis is common but not irreversible. It begins subconsciously, and fat accumulates in the liver slowly but surely. But ignorance is bliss. Performing the right act—weight control, dietary restriction, exercise, abstention from food and drugs under a physician’s guidance—can restore the liver to its natural state.
It’s not a liver disease. It’s about protecting your energy, your heart, and your life. Act early, and you can turn the page in your health book. Your liver will pay you back with years of vitality and quiet effort.